On Wednesday, February 7, over 150 people gathered for the Music in Health Care symposium—a one-day series of presentations and panels hosted by the Center for Performing Arts Medicine (CPAM) focusing on the various uses of music in health care.
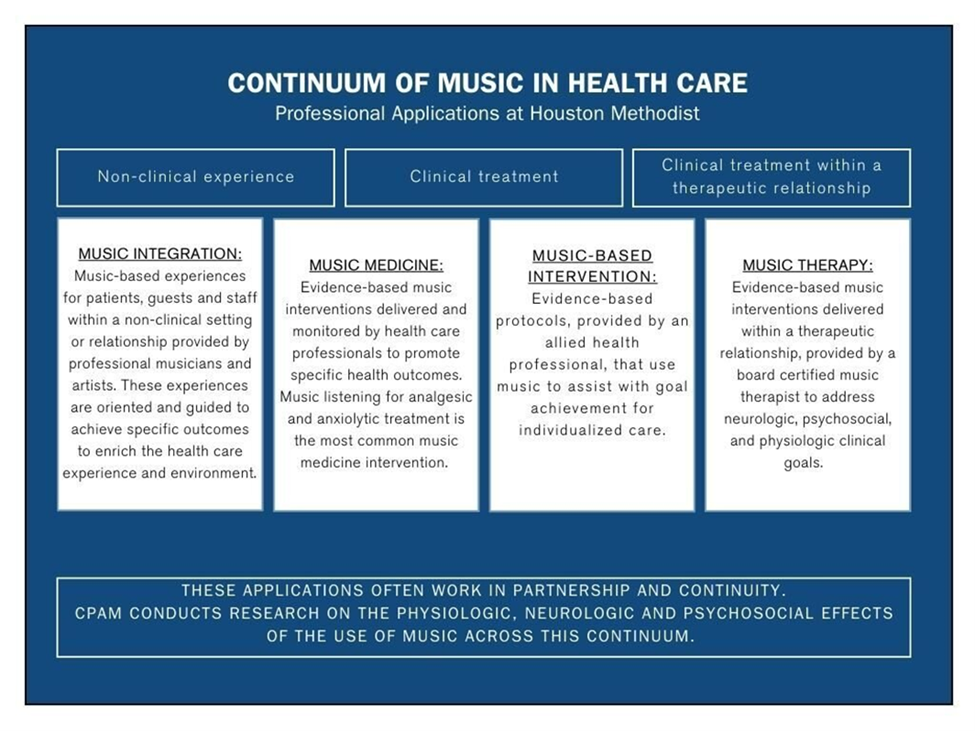
Attendees were greeted by the tranquil melodies of guitarist Jimmy Smith as they arrived at the event. Following this, CPAM creative arts therapy manager Jennifer Townsend and CPAM clinical educator Virginia Gray. The goal of the symposium, they said, is to illuminate the distinctions between music medicine, music therapy, and music enrichment. Attendees were encouraged to engage with a continuum developed by CPAM that serves as a visual representation of the ways music can be harnessed in the health care setting as defined by CPAM’s current work.
Keynote speaker Suzanne Hanser participated in an interview-style keynote speech with questions asked by Jennifer Townsend. Hanser explored the importance of defining music in the health care setting, ethical considerations of using music in health care environments, and the direction of the music therapy field. “We need to define what we do,” Hanser said. “Music is a powerful tool, and there are many contraindications.” That is why it is important to understand music’s impact and each health care provider’s role.
“Knowing the literature and knowing the contraindications as well as understanding your scope of practice is part of ethical practice,” Hanser said. “It’s also ethical practice to know when music is medically necessary.”
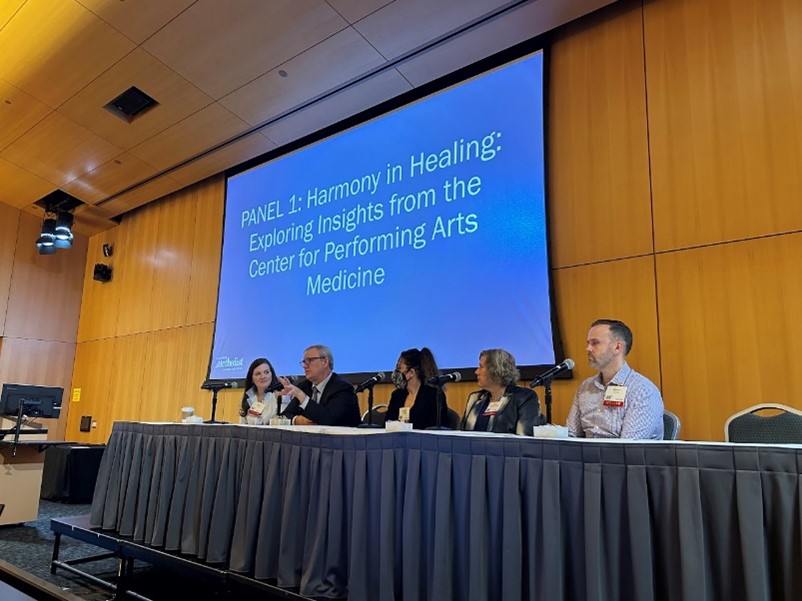
Next, a panel consisting of CPAM staff members from the creative arts therapies, research, and arts integration departments discussed how CPAM’s projects work together, as well as how different modalities can collaborate to promote well-being in various health care environments. Todd Frazier highlighted different entry points for patients to engage with the arts throughout the hospital, such as pianists playing in the lobby, the art cart visiting patient rooms, and creative arts therapists providing services. The panelists agreed that it is important to “know the research”—to be informed by evidence and literature that show the effectiveness of these arts-based interventions.
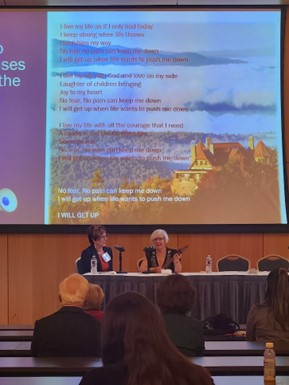
Music therapists Ashley Lundquist and Sarah Rossi presented Voices Echo, where they presented an album written by patients undergoing the cancer treatment journey. They explored the songwriting and recording process of the album as well as their goal of enhancing the well-being of both patients and staff. By participating in the album via songwriting, listening, or sharing, patients and staff members engaged in reinforcement of healthy coping strategies and validation of various emotions throughout the cancer treatment journey.
Chaplain Brian Gowan shared Newborn & Parents Blessing Song Video, a music video created by sixty Houston Methodist staff members that he shares with new patients and staff. The music video gave staff members the opportunity to engage with the fine arts and provide a resource for future patients. Gowan shared that he uses music regularly in his practice to establish connections and validate emotions.
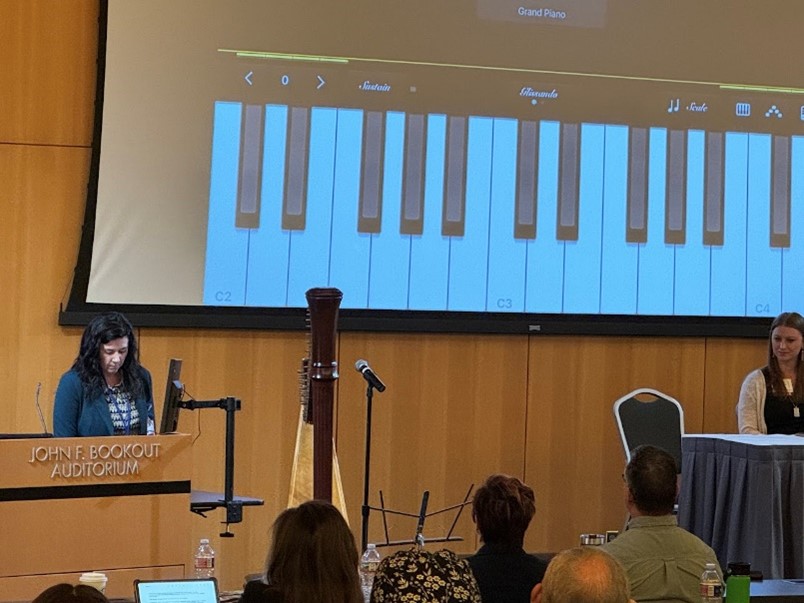
Music therapist Mary Kate Becnel led an interactive session that demonstrated how GarageBand can be used to support and enhance the songwriting process. Her walkthrough showed how loops, MIDI, recording, and FX features can be easily used in GarageBand to create a song. “It’s a music therapist’s benefit and challenge to work to make music that’s accessible to everyone regardless of musical experience,” Becnel said.
Artist in residence Emily Klein and recreational therapist Stephanie Janczak presented the benefits of having an artist in residence regularly visit a unit. They highlighted positive feedback and responses from patients and role-played the scenario of an artist in residence interacting with a patient. Emily and Stephanie work together to determine a patient’s musical preferences and support the patient’s treatment goals.
After lunchtime, during which pianist Dehner Franks provided live music, a poster session was held. Topics of the presentations included environmental music therapy, the use of music in end-of-life care, an artist in residence, patient satisfaction outcome measures, an employee choir, a music therapy and art therapy collaboration, neonatal music therapy, and music medicine.
Next, a panel consisting of various medical providers navigated the impact of music on health care. Dr. Atiya Dhala shared that she began using music with patients as a way of providing more holistic care for their well-being, and she emphasized the importance of the evidence base for music’s role in health care. “It’s well published that music, used as positive stimulation, leads to reduction in stress hormone levels and heart rate. There’s a lot of data on that,” Dr. Dhala said.
Dr. Ben Renfrow spoke enthusiastically about being introduced to music therapy through the work of music therapist Maegan Morrow and advocated for bringing more attention to the music therapy profession. “All of the students that come to work with the different disciplines in our department are now getting exposure to music therapy and they can be advocates for that,” Dr. Renfrow said. “Once they have that exposure, it’s hard to go without it.”
Todd Frazier presented a study that highlighted how directed music listening impacted the brains of stroke recovery patients. “This is an example of music medicine collaborating with music therapy. It’s also a prime example of how we can harness the potential of music individually to be used as a medicine to help in recovery,” Frazier said. Music was shown to be effective in stimulating different areas of the brain compared to non-music, and there was a difference between familiar and unfamiliar music. Frazier said that this research, along with other research studies conducted by CPAM, is crucial and impactful. “We pride ourselves on trying to be translational; what we do can immediately be translated to practice,” Frazier said.
Dr. Riya Bhavsar presented on ways that music therapy can be used in stroke rehabilitation. She highlighted Neurologic Music Therapy, a field of music therapy that focuses on physical and cognitive rehabilitation, and provided examples of music therapy techniques at work in working with patients in domains such as verbal communication and physical motor movements.
Mehjabeen Momin and Dr. Pinky Shani presented a study on how music medicine was used in the Post Anesthesia Care Unit (PACU) for patients who had undergone abdominal surgery in general anesthesia. Music was shown to help decrease reported levels of anxiety and pain, and it decreased patients’ length of stay in the hospital.

Art therapist Addy Purdy and music therapist Jessica Hernandez shared about how music therapy and art therapy work in close collaboration on the Houston Methodist inpatient psychiatrist unit. The music therapist and art therapist co-lead groups together and facilitate Open Studio, a time when patients can come in and participate freely in art- or music-making. The collaborative goals of this treatment include encouraging creative self-expression, exploring and processing emotions, promoting mentalizing, and enhancing insight into—and developing supportive tools in response to—experiences and behaviors. They highlighted the value of having music therapy and art therapy work in tandem: doing so allows patients access to more resources, creates potential for deeper and faster changes, allows for more holistic treatment and better data collection, and provides beneficial learning opportunities among clinicians.
CPAM’s chairman, Dr. Robert Jackson, provided closing comments to round out the day. Dr. Jackson said he has been a firsthand witness to the transformative impact of music on health, and music has proven itself to be a therapeutic force. He referenced the long history of music’s use as a healing tool and the founding of CPAM to serve artists in the community.
“The symposium is not an end but a stepping stone toward a future where music and health care walk hand in hand,” said Dr. Jackson.