Marissa Salinas is a music therapist who works at Houston Methodist Baytown. In this spotlight, spend a day with Marissa as she provides music therapy to patients on the intensive care units (ICU) and intermediate care units (IMU).
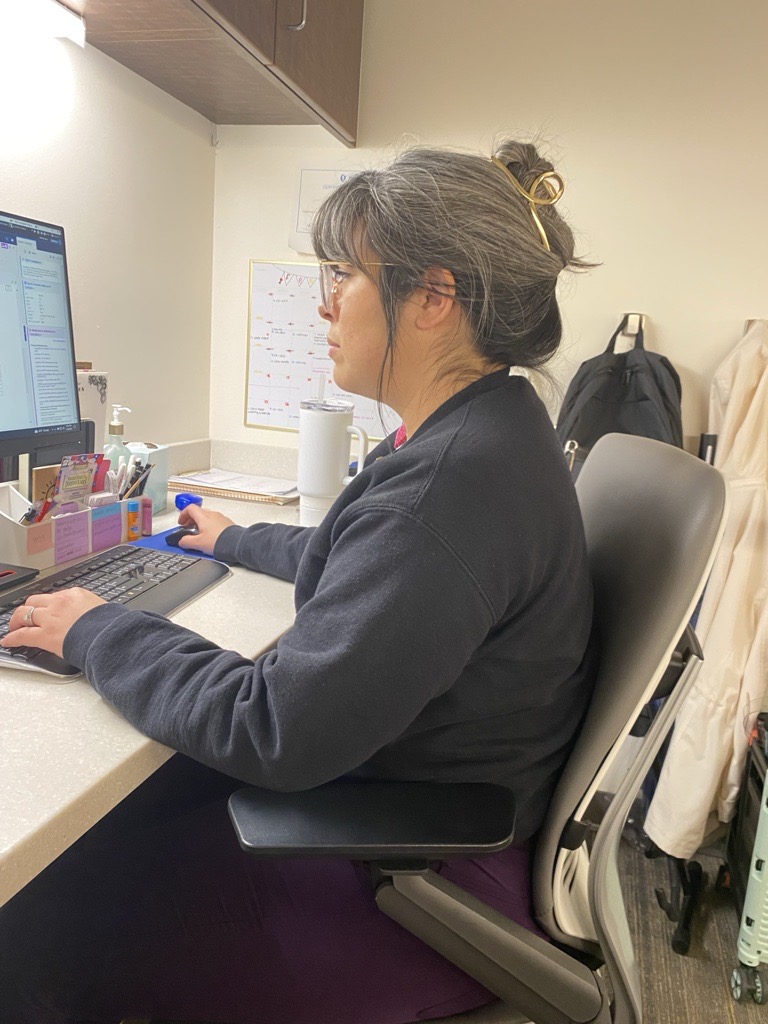
Marissa begins her work day at 7:30 AM with what she calls her “office hours”—time spent reviewing updates from her current list of patients, receiving new referrals, and making resources such as visuals and handouts for her patients.
At 10 AM, Marissa attends rounds on the ICU. During rounds, the treatment team gathers to share the latest medical information on every patient on the unit. Marissa listens for patients with medical goals related to delirium, sedation, and ventilator liberation support. If a patient is experiencing delirium, is sedated, or is on a ventilator, Marissa wants to know, because the patient may be a good candidate for music therapy. Positive stimulation such as music has been shown to help with addressing delirium, and music therapy can help with preventing and reducing its symptoms. If a patient is on the ventilator—or the “vent”—then Marissa may be able to help with vent liberation, which is when the patient’s use of the ventilator is gradually reduced. Other things may indicate a patient may be a good referral for music therapy, such as anxiety, upcoming hospice care, and mobility goals.

Over the next few hours, Marissa engages patients in music therapy sessions. She brings instruments, songs, resources, and other materials that may help patients meet their treatment goals. Generally, Marissa provides live music rather than recorded music, since live music can be adjusted in real time to meet patients’ needs.
Marissa’s assessment of a patient begins before she even walks in the door and continues throughout the session. She gathers information about each patient by reviewing their chart, asking questions to them and/or their family members, and talking with the patient’s treatment team members. This information helps her formulate treatment goals for her patients and choose music that is individualized to each person’s treatment goals and preferences.
During treatment, Marissa uses a chart she created to record patients’ vital signs, such as their heart rate and blood pressure, and other measures of their progress, such as their pain and anxiety levels before and after each session. These measures help show the effectiveness of music therapy treatment and help the treatment team see patients’ progress.
Marissa usually brings her iPad, which is held up by an iPad stand and can be used to display or organize music. She uses the guitar in most sessions, depending on the patient’ needs and preferences. During the session, she may talk with the patient and/or their family members or provide music to meet certain goals. Music may be used as distraction from nausea, or it may be timed with someone’s rhythmic gait to help them improve their walking ability. Marissa may sing songs with lyrics or musical elements that validate or reflect emotions expressed by a patient grappling with a poor prognosis or by a patient about to undergo a stressful procedure.
In one session, Marissa sang songs George Strait’s “Amarillo by Morning” and John Denver’s “Take Me Home, Country Roads” to a patient who enjoys country music . She provided music as positive stimulation to distract from the patient’s pain levels, which the patient rated 9 out of 10. She matched the musical elements to the patient’s pain state, then gradually adjusted the music to try to decrease the patient’s pain perception. During the session, they talked about the patient’s family, the patient’s upbringing, and the patient’s use of music. By the end of the session, the patient showed a livelier expression and expressed appreciation for Marissa’s visit.
After music therapy sessions, Marissa updates the patient’s treatment team through progress notes documented in the electronic medical record system and by talking to the patient’s team members, such as their nurse. Marissa documents immediately after sessions to ensure that she accurately captures what happened during the session. Progress notes capture when sessions took place, what happened during the session, and what treatment recommendations Marissa has for the patient. This can take a while, as a significant amount of information can be captured in a single session. A patient’s words and musical preferences may be documented for future sessions. Signs of patient progress may also be captured; a patient experiencing anxiety may show more relaxed body language by the end of a session, or a patient who had been failing spontaneous breathing trials may perform better with music therapy treatment. The vital signs Marissa captured at the start and end of the session may also be useful in understanding the patient’s response to music therapy treatment.
Marissa’s job responsibilities are not limited to patient care. She also works to provide education to team members who may not be aware of music therapy or its clinical benefits. When talking to other staff at the hospital, Marissa defines music therapy and talks about how it can be used to help patients meet their goals. She also gives presentations geared toward staff members that provide examples of music therapy.
Marissa usually visits patients until around 3 PM. To wrap up the day, she finishes documenting her sessions, creates activities and other resources for patients, and makes plans for the next day. Sometimes she spends this time reading the latest research on music therapy findings or responding to emails that came in while she was seeing patients.
Although the days vary, Marissa’s goal is always the same: treating and caring for the “whole person” while embodying Houston Methodist’s I CARE values (integrity, compassion, accountability, respect and excellence).
“I’ve been blessed to have made an impact on many lives while serving at Houston Methodist, including my patients, their loved ones, my coworkers, and my own loved ones”, says Marissa.